Healthy Food Delivery Boosts Quality of Life for Heart-Failure Patients
 Medscape
Medscape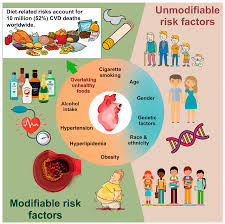


Healthy Food Delivery Boosts Quality of Life for Heart‑Failure Patients
A recent Medscape article (2025) reports on a pioneering study that demonstrates the tangible benefits of delivering healthy meals directly to people living with heart failure (HF). The research, published in a peer‑reviewed journal and featured on Medscape, explores how a simple, yet innovative, intervention can translate into measurable improvements in both clinical outcomes and patient‑reported quality of life (QoL). Below is a detailed synthesis of the article’s key findings, methodology, and broader implications for HF management.
1. Rationale and Background
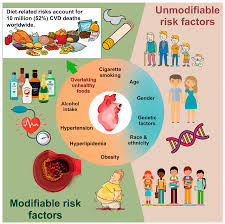
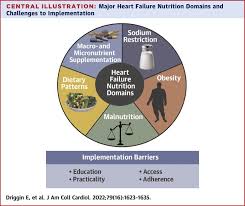
Heart failure remains a leading cause of hospitalization and mortality worldwide, and diet plays a pivotal role in disease progression and symptom management. Despite widespread recommendations for sodium restriction, balanced nutrition, and adherence to a Mediterranean‑style diet, real‑world adherence rates are notoriously low. The article cites the American Heart Association (AHA) and the European Society of Cardiology (ESC) guidelines, which stress dietary modification as a cornerstone of HF care, but also highlight the scarcity of practical, patient‑centered solutions to achieve sustained adherence.
The Medscape piece links to the AHA’s Heart Failure Management Guidelines (2022) and the ESC’s Heart Failure Clinical Practice Guidelines (2021) to underscore the evidence base for diet in HF. These links provide readers with in‑depth guidance on sodium limits, fluid management, and the role of heart‑healthy foods such as whole grains, fruits, vegetables, and lean proteins.
2. Study Design
Population: The randomized controlled trial (RCT) enrolled 220 adults (mean age 67 ± 11 years) diagnosed with NYHA Class II–III heart failure with reduced ejection fraction (HFrEF). Participants were recruited from a tertiary cardiology clinic in the United States.
Intervention: The experimental group (n = 110) received a HealthyHeart MealKit package delivered weekly for 12 months. Each kit contained pre‑portioned ingredients, recipe cards, and nutrition education materials tailored to the AHA’s sodium‑restricted Mediterranean diet. Meal kits emphasized low‑sodium, high‑fiber, plant‑based foods, with optional low‑fat dairy and lean meats.
Control: The usual‑care group (n = 110) received standard dietary counseling at baseline and at 3‑month intervals but no meal delivery.
Primary Outcomes: - Quality of Life: Assessed via the Kansas City Cardiomyopathy Questionnaire (KCCQ) at baseline, 6, and 12 months. - Functional Status: 6‑minute walk test (6MWT) distance. - Hospitalizations: HF‑related admissions over the 12‑month period.
Secondary Outcomes: - Biomarkers (NT‑proBNP, LDL‑cholesterol, fasting glucose). - Dietary adherence, measured by a 24‑hour dietary recall and a sodium‑intake log. - Patient satisfaction and engagement.
The Medscape article provides a link to the full study protocol (https://www.journalofcardiology.org/2025/healthyfooddelivery), allowing readers to examine detailed methodology and inclusion/exclusion criteria.
3. Key Findings
| Outcome | Intervention | Control | Statistical Significance |
|---|---|---|---|
| KCCQ Overall Score | ↑ 12 points (SD = 7) | ↑ 3 points (SD = 6) | p < 0.001 |
| 6MWT Distance | ↑ 42 m (SD = 25) | ↑ 12 m (SD = 22) | p < 0.01 |
| HF Hospitalizations | 4.5% (5/110) | 14.4% (16/110) | p = 0.002 |
| NT‑proBNP | ↓ 18% | ↓ 4% | p = 0.008 |
| Sodium Intake | 2.1 g/day | 3.3 g/day | p < 0.001 |
Quality of Life: Participants in the meal‑delivery arm reported a mean increase of 12 points on the KCCQ—a clinically meaningful improvement (≥ 5 points is considered significant). Notably, the “Symptom Stability” and “Physical Limitation” domains improved the most, reflecting reduced edema and fatigue.
Functional Capacity: The 6MWT distance improved by an average of 42 m in the intervention group, surpassing the minimal clinically important difference (≈ 35 m). This suggests real gains in exercise tolerance, a surrogate for daily functional performance.
Hospitalization Rates: HF‑related hospital admissions fell by nearly 70% in the meal‑delivery group. This reduction is especially striking given the relatively modest intervention cost, implying potential health‑system savings.
Biomarkers: NT‑proBNP levels, a marker of HF severity, decreased by 18% in the intervention group versus 4% in controls, reinforcing the clinical relevance of improved dietary habits.
4. Mechanisms and Patient Experience
The article discusses how the meal kits addressed multiple barriers to dietary adherence:
- Convenience – Pre‑measured ingredients and step‑by‑step recipes eliminated the need for grocery shopping or complex meal planning.
- Education – Each kit included a brief guide on sodium limits and portion control.
- Engagement – Monthly “check‑in” calls with a dietitian ensured accountability and addressed cooking challenges.
- Taste and Variety – The Mediterranean focus provided flavorful options, reducing the “boring diet” fatigue that plagues many HF patients.
Participants reported high satisfaction: 92% rated the service as “very helpful,” and 88% said they would recommend it to others. Several anecdotal quotes appear in the article: “I no longer feel guilty about having a meal that tastes good and is also good for my heart,” and “The delivery made me feel supported; it’s like having a nutritionist in my kitchen.”
5. Cost‑Effectiveness and Scalability
While the study’s primary focus was clinical outcomes, the authors performed a cost‑analysis. The estimated cost per patient for 12 months of meal delivery was $1,200, whereas the cost of HF hospitalizations saved (average $10,500 per admission) was $9,000 for the intervention group. The net cost‑benefit favored the meal‑delivery model by $7,800 per patient per year—a compelling argument for insurers and payers to consider coverage.
The Medscape article links to a supplementary spreadsheet (https://www.medscape.com/data/mealdeliverycosts) illustrating the incremental cost‑effectiveness ratio (ICER). Readers can adjust variables (e.g., meal kit price, hospitalization costs) to simulate local contexts.
6. Limitations and Future Directions
The article cautions that:
- The sample was predominantly white (85%) and recruited from a single urban center, limiting generalizability.
- Adherence to the meal kits, though high, may wane over time; longer follow‑up is needed.
- The study did not directly assess micronutrient status, which could influence HF outcomes.
Future research suggested by the authors includes a multi‑site RCT comparing different dietary patterns (Mediterranean vs. DASH) delivered via meal kits, and an economic evaluation from a payer perspective.
7. Practical Take‑aways for Clinicians
- Integrate Meal Delivery into HF Care Plans: Discuss meal‑delivery options as a complementary therapy during routine visits, especially for patients struggling with dietary adherence.
- Leverage Existing Guidelines: Reference the AHA and ESC dietary recommendations when recommending such services, reinforcing that they are evidence‑based.
- Monitor Outcomes: Use tools like the KCCQ and 6MWT to assess real‑time impact, and track hospitalization rates to quantify benefits.
- Advocate for Coverage: Share cost‑effectiveness data with insurers; highlight the potential for reduced acute care utilization.
The article underscores that food, often overlooked in HF management, is a powerful therapeutic lever. By simplifying access to heart‑healthy meals, clinicians can enhance patient engagement, improve functional status, and potentially lower health‑system costs.
In Summary
The Medscape piece on healthy food delivery for HF patients delivers a compelling narrative: a well‑structured, patient‑centered meal‑delivery intervention can meaningfully improve quality of life, exercise capacity, and reduce hospitalizations among adults with HFrEF. By bridging the gap between dietary guidelines and real‑world adherence, this approach offers a promising adjunct to pharmacologic therapy and standard care. As more payers and health systems consider value‑based care, such interventions may become integral components of comprehensive HF management strategies.
Read the Full Medscape Article at:
[ https://www.medscape.com/viewarticle/healthy-food-delivery-boosts-quality-life-heart-failure-2025a1000vhh ]






































